On the last day of September, the constantly-changing microbial world proved its power to deliver surprises and shocks.
Within 24 hours, three deadly diseases surfaced again, twice in unheard of places. Austria confirmed its first imported case of Middle East Respiratory Syndrome. Egypt confirmed a case of H5N1 avian influenza in an infant. And the United States confirmed its first case of Ebola virus disease in a Liberian traveller to Dallas, Texas. That case proved fatal. The other two patients remain seriously ill.
Meanwhile on that same day, more than 90 Ugandans -- most of them hospital staff -- were being monitored, in isolation, following the death on 28 September of a radiology technician from yet another horrific killer: Marburg hemorrhagic fever.
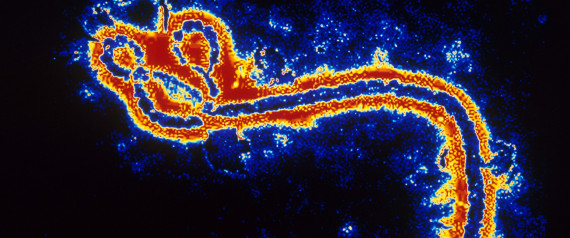
Of all these events, the outbreak of Ebola virus diseases that is ravaging parts of West Africa poses the greatest threat to international security, as confirmed last month by an emergency session of the UN Security Council.
Ebola has no proven vaccines or treatments. The World Health Organization (WHO) has responded to the urgent need for containment measures that go beyond the status quo: isolation and basic supportive care. In the view of WHO and many others, ways must be found to prevent this disease and lower the current fatality rate, estimated at 60 percent to 70 percent.
With this goal in mind, WHO is evaluating new and unregistered vaccines and therapies, together with the possible use of treatments already registered for managing other conditions.
Testing the most promising vaccines -- the fastest trials in history
Vaccination is the ideal intervention in this outbreak. It offers the best long-term protection for at-risk populations in the most cost-effective way. Two of the most promising vaccines are already in phase I, or "safety," clinical trials.
In an expression of solidarity with the people of West Africa, these trials, in healthy human volunteers, are being conducted in the U.S. and the United Kingdom as well as in Mali. Germany, Switzerland, Gabon, and Kenya will follow shortly.
And the news keeps getting better: phase II trials will be rolled out to provide both safety and efficacy data in affected countries and their neighbors within the next three to six months. Never before has the R&D community moved so fast, without compromising international standards for testing new medical products. The objective: to give the African people the best vaccine that the world's scientific community, working together in overdrive, has to offer.
Blood and blood-derived therapies
Whole blood transfusions from recovered patients have been used, with some suggestions of efficacy, since as far back as 1976, when the Ebola virus first emerged in almost simultaneous outbreaks in Central Africa.
Therapies using both whole blood and plasma derived from recovered patients are judged by WHO to be feasible treatment options -- even within the severe resource constraints faced in each of the three countries. Blood therapy has already been used in just a few patients infected during the current outbreak. If upcoming efficacy trials in each of the three countries produce positive results, these therapies could be rapidly scaled up to treat many.
The use of convalescent plasma (a component of whole blood) is a second treatment option, but requires much more technical and practical support to ensure safety and good quality management. Other blood products, such as immunoglobulins, are being investigated under the guidance of WHO.
The state-of-the-art with experimental medicines
Multiple experimental medicines are in the development pipeline. While studies in animal models have been encouraging, none of these products has been proven to be either safe or effective in humans.
Most have one major drawback: extremely small quantities; in the case of ZMapp -- the best known -- supplies are said to be exhausted.
Other potential medicines are limited by concerns about their possible side-effects. Some could prove to be toxic at the high doses needed to turn the clinical course around.
At present, WHO is systematically gathering, analyzing, and communicating to doctors and industry all data generated by the use of such medicines to treat Ebola patients in the current outbreak.
Some drugs already licensed to treat other conditions are also being investigated for their effectiveness in reducing disease severity and the unacceptably high fatality rate. The big advantage of licensed products: their safety has already been demonstrated.
All such evaluations need to take place in a context of good-quality supportive care to ensure that patients are adequately hydrated and have the right balance of electrolytes. The severe diarrhea and vomiting characteristic of this disease significantly disrupt some vital bodily functions.
Diagnostics
WHO is also prompting the scientific community to address another urgent need: for point-of-care diagnostic tests that can be used in overflowing treatment centers. By speeding up and streamlining safe and accurate diagnosis, medical staff can do a better job of keeping suspected Ebola patients separate from patients who may be suffering from any of many long-tenured infectious diseases -- from malaria and typhoid fever to Lassa fever, dengue hemorrhagic fever, and yellow fever -- that constantly plague these three countries.
Is all this ethical?
Yes. A WHO consultation in mid-August determined that, in the midst of the present crisis, it was both ethical and desirable to use unregistered drugs and vaccines immediately -- even in the absence of safety and efficacy data compiled in humans. However, the experts insisted on adherence to certain clear standards of evidence, whereby studies in relevant animal models bring at least some confidence that use in humans will be clinically beneficial.
Ethical considerations are a fundamental part of intervention selection and of clinical trial design. In the context of the current outbreak, with its extreme case-fatality rate and complex social dynamics, conventional approaches to clinical trials might be inappropriate, unworkable, and surely way too slow. Several innovative trial designs are now being pursued.
No stone left unturned
While many difficult scientific issues remain to be resolved, one thing is clear: WHO and its scientific and industry partners are making sure that no stone is left unturned, that no international standards for safety and quality are compromised.
This is a powerful expression of support for the people of West Africa. A humane world cannot let these people suffer on such an extraordinary scale.
